 If you know that weight loss surgery is for you, you may have questions about the type of surgery that would best help you reach your health and weight loss goals.
If you know that weight loss surgery is for you, you may have questions about the type of surgery that would best help you reach your health and weight loss goals.
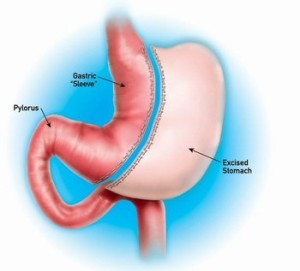
Of the weight loss surgeries currently available, gastric sleeve, or sleeve gastrectomy, is a safe choice with less side effects than other types that transitions well into later surgeries if need be. But how does this popular procedure work?
Gastric Sleeve Basics
A sleeve gastrectomy is performed laparoscopically using a small incision. Through the incision, your surgeon will insert a viewing tube attached to a tiny camera, as well as small instruments, to help remove 85 percent of the stomach and form a tube or sleeve that serves as your new digestive pouch. He then staples this pouch shut.
Patients wishing to “tweak” their results can follow up this surgery with a gastric bypass procedure or duodenal switch surgery, both of which are safer to perform after undergoing the sleeve gastrectomy. By “staging” subsequent surgeries in this way, usually 18 months after the initial gastric sleeve surgery, patients are able to lose more weight by the time of the second procedure and can physically adjust to the surgical changes in a more gradual – and healthy – manner.
The Benefits
Gastric sleeve surgery has inspired leagues of fans who swear by its results. The following are the most common benefits of a gastric sleeve procedure:
- Reduced hunger sensations and stomach capacity so that patients feel fuller faster and automatically eat less.
- Intact digestive tract, allowing for normal digestion and absorption of nutrients.
- Does not involve the implantation of a medical device, such as a gastric band.
- Can usually be performed laparoscopically regardless of a patient’s weight.
- Viable option for patients with medical issues that disqualify them from undergoing other type of weight loss surgery.
- Can be used as part of a staged process in which patient plans to undergo a duodenal switch or gastric bypass at a later date.
- Provides the option to revise surgery for those who already have an adjustable gastric band.
- Overall, the smaller incision, lack of gastric banding, and intact digestive tract make this procedure particularly appealing.
The Risks
No surgery comes without risks. Despite being one of the safest weight loss surgeries available today, gastric sleeve procedures can include the following:
- Leaking of the sleeve: If the staples holding the sleeve closed do not hold, leaking stomach acids can create infection of nearby tissues and may require another operation to correct.
- Blood clots
- Regain of weight over time due to stretching of the sleeve.
Your best chance of avoiding complications during your gastric sleeve procedure is to work with a team that is known for its low mortality and complication rate. Look for programs with a comprehensive approach to surgery, involving extensive dietary coaching and support groups to help you stay on track after the procedure. Attend a few seminars before choosing your program to help you decide what team will best encourage your success.
How will my life change?
As with any weight loss surgery, a sleeve gastrectomy requires physical, mental, and emotional adjustments. Be sure to discuss these changes with those closest to you so that they will be prepared to support your new lifestyle, post-op and beyond.
Post-op
Immediately following your surgery, you will likely have some belly and incision pain and may wish to use pain medication, at least for the first 24 hours. Your stomach is now substantially smaller, and you will feel full quicker as you eat. You may also experience a phenomena called “dumping syndrome,” in which food that has been consumed empties too rapidly into your small intestine. While this syndrome is more common in patients who have experienced intestinal re-routing through a Roux-en-Y surgery, dumping syndrome can occur in gastric sleeve patients.
Dumping syndrome can make patients feel faint and shaky and can prompt an episode of diarrhea. Physicians advise that patients looking to avoid dumping syndrome refrain from consuming refined sugars, which rapidly absorb water from the body, as well as dairy products and deep fried foods.
Diet
Your post-operative diet adheres to specific instructions from your doctor. During your first month, you will focus on consuming only small amounts of soft food and liquid. Keep a water bottle handy and sip often to remain hydrated, which will help with constipation, a common side effect.
Under the guidance of your doctor and dietician, you will gradually be able to add solid foods back into your diet. It is vital to eat slowly and focus on chewing each bite before swallowing. Metered eating helps prevent dumping syndrome and allows you to savor the small amounts of food that you do consume, as well as prevent nausea and vomiting.
Social Changes
Because food is a major part of many social functions, be prepared to adhere to your doctor-approved diet no matter what those around you are eating. While sticking to a bariatric diet can be a challenge in the best of circumstances, the benefits of staying true to your plan far outweigh the hardship of not eating what your peers do. Avoid temptation and potential discomfort by discussing your diet with your hosts in advance, and with any trustworthy friends in attendance who didn’t get the weight loss surgery memo.
Words to the Wise
Undergoing any type of surgery is a serious decision and should not be taken lightly. In addition to changes in the amount of food you now consume, your new body requires that you prioritize only the most nutritious foods to be sure that you are still consuming all the nutrients you need.
High-calorie liquids may prevent weight loss, so stick with water and low-calorie juices. Also, be wary of carbonated beverages, as they can cause uncomfortable gas during the first few months.
Your goal is for your surgery to “take” and continue to help you meet your goals for years to come. Even if you are staging your weight loss with multiple surgeries, you want your gastric sleeve surgery to provide sustainable weight loss. Overeating is a big no-no and can undermine the effectiveness of your surgery by stretching the size of your smaller stomach over time. Focus on small meals, consumed slowly.
Finally, remember that weight loss surgery of any kind is no guarantee of long term weight loss. Regular exercise and behavior modification to target negative habits where they start – in the mind – will be necessary parts of your weight loss journey, no matter what surgery you choose.
Sounds great, but do I qualify?
Qualification for a gastric sleeve procedure is similar to qualification for other weight loss procedures. The National Institutes of Health (NIH) requires patients to have a body mass index (BMI) greater than 40 to qualify. Those with obesity-related illnesses and BMIs ranging from 35 to 39 are also excellent candidates. Regardless of your BMI, if you are coping with excess weight that seems impossible to lose and negatively affects your health, it is worth your time to have a discussion with your doctor about your options, surgical or otherwise.
Even if you do qualify for a gastric sleeve procedure on paper, getting your surgery covered by insurance can be a challenge. For information on the financial side of weight loss surgery, check out our recent blog post.
Undertaking weight loss surgery is a life-changing choice. A sleeve gastrectomy will change the way you eat, exercise, and relate to your body. With the right information, you can make empowering choices that lead you toward your goals and improve your health and confidence along the way.
